
VHF Safety Clothing for Frontline Caregivers During a Viral Hemorrhagic Fever Outbreak
Most people have heard of Ebola virus. First discovered in 1976, the deadly virus made international headlines in 2014 through 2016, when an outbreak spread from West Africa and within months progressed into a global epidemic.
More recently, the World Health Organization (WHO) announced two fatal cases of Marburg virus disease in Ghana—a viral outbreak which the WHO warned could "represent a serious public health threat as it is severe and often fatal."
Marburg virus, Ebola virus, and many others cause deadly infectious diseases called viral hemorrhagic fevers (VHFs). Due to the highly infectious and often-fatal nature of these diseases, all VHFs must be treated with specific guidelines and safety precautions—not the least of which is the proper type, use, and disposal of personal protective equipment (PPE).
For this reason, the Occupational Safety and Health Administration (OSHA) and other governing bodies have created strict PPE and safety protocols that healthcare personnel must follow, not only to protect themselves but also to slow and prevent the spread of infection.
In this article, we learn about what VHFs are and the viruses that cause them, signs and symptoms of viral hemorrhagic fever, prognosis, long-term outcomes for people with VHF, and in-depth information on the type of VHF safety clothing and precautions that should be utilized when caring for people with suspected or confirmed cases of VHF.
What Viruses Cause Hemorrhagic Fevers?
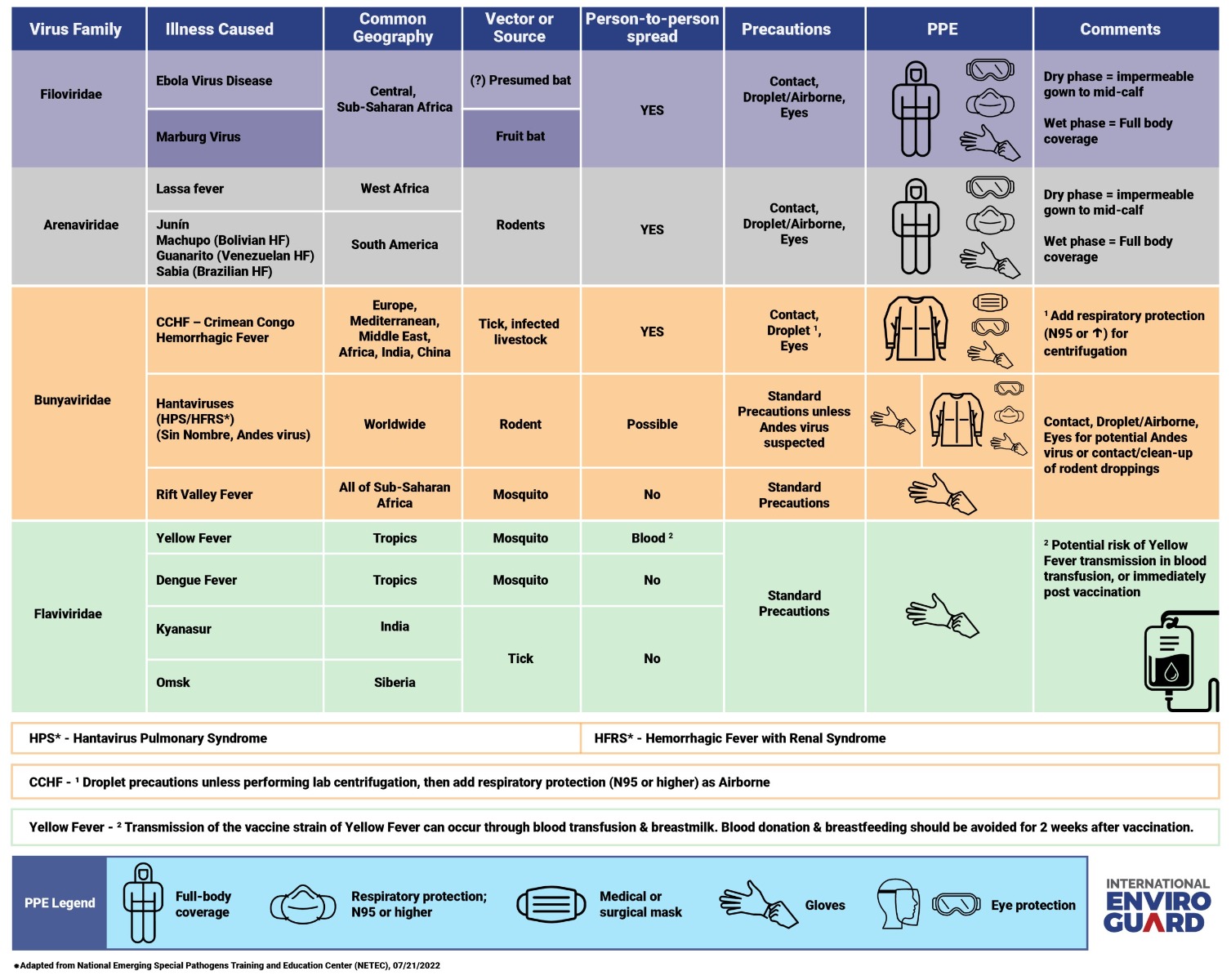
Viral hemorrhagic fevers are caused by a group of viruses which come from four distinct viral families. The four viral families known to cause VHFs include:
- Filoviridae, which includes the Ebola and Marburg viruses
- Arenaviridae, which includes the Lassa, Junin, and Sabia viruses
- Bunyavirales, which includes Nairovirus, known for causing a disease called Crimean-Congo hemorrhagic fever
- Flaviviridae, which includes the Yellow Fever and Dengue viruses
Despite belonging to distinct viral families, all viruses that cause VHFs share several common features and characteristics, according to the Centers for Disease Control and Prevention (CDC):
- They contain genetic material known as ribonucleic acid (RNA), which can change quickly over time
- They are encased by an outer layer of lipoprotein (molecules made of protein and fat) and therefore are easier to destroy with physical and chemical methods (e.g., heat, sunlight, bleach, detergents, solvents)
- Their natural hosts are animals (e.g., monkeys) and insects (e.g., ticks) and are generally restricted to geographical areas where the host animals live
- They are zoonotic, meaning they can spread from an infected animal or insect to a person—and some can then spread from person-to-person (the specific route of viral transmission is exposure to bodily fluids or excretions of infected organisms, including blood, urine, feces, vomit, and respiratory droplets)
The CDC also warns that VHF outbreaks in people are considered difficult to prevent because they tend to be unpredictable and sporadic. Complicating the matter is that testing and treatment options for VHFs are limited, and accurate diagnosis often takes time.
What Are the Common Characteristics of a Hemorrhagic Fever?
Viral hemorrhagic fevers affect multiple organ systems within the human body. While some VHFs cause relatively mild illnesses, others can lead to severe and potentially life-threatening complications. How long it takes for a person to start showing symptoms of VHF after becoming infected depends on the specific virus but can range from a few days to a few weeks.
Some of the most common signs and symptoms of VHFs include fever (body temperature > 38°C/100.4°F), severe headache, dizziness, skin rash, muscle and/or joint pain, diarrhea, nausea, vomiting, and fatigue. Infection with certain viruses can lead to additional concerns, such as thrombocytopenia (decreased platelets in the blood), jaundice, weight loss, bleeding from the eyes, ears, or mouth, inflammation of the throat, protein in the urine, and chest pain.
In severe cases, VHF can lead to fatal consequences including respiratory distress, delirium, internal bleeding, organ failure, shock, coma, and death.
The Health Effects and Prognosis of Hemorrhagic Fever
According to the U.S. National Library of Medicine, viruses that cause VHFs replicate rapidly inside the host animal or person. This viral replication can trigger a powerful immune response that can lead to systemic issues including increased vascular permeability (blood vessels become "leaky"), abnormal blood clotting, and immune cell death. Virtually all systems within the body can be impacted by a VHF, including the cardiovascular and nervous systems.
Are Viral Hemorrhagic Fevers Survivable?
Survival statistics for viral hemorrhagic fever vary widely and depend largely on the type of virus implicated. Generally speaking, case-fatality rates can range from less than 10 percent to as high as 90 percent, particularly in developing countries.
While these infectious diseases can be mild and fully recoverable, some survivors of VHF struggle with long-term health complications including fatigue, deafness, and organ damage. Currently, there is no known cure, vaccine, or specific treatment for viral hemorrhagic fevers. The focus of treatment is largely about managing symptoms and minimizing complications.
Recommended VHF Protective Clothing for Frontline Healthcare Workers
Early diagnosis of VHF (and appropriate use of VHF protective clothing!) is essential to protect patients, healthcare workers, and communities at large. We've learned, however, that early diagnosis can be difficult, especially since VHFs often present like other illnesses like malaria or human immunodeficiency virus (HIV). The following algorithm may help personnel on the frontline:
- Identify: consider a person's symptoms, travel history, and exposure history and initiate all necessary precautions as soon as a patient is suspected to have VHF
- Isolate: follow all regulatory guidelines regarding patient quarantine/isolation, PPE use, caregiver roles and responsibilities, and other factors that are relevant to your organization's specific administrative, environmental, and engineering constraints
- Inform: immediately alert the appropriate stakeholders (including your organization's infection control team and local health department) of any suspected or confirmed VHF cases
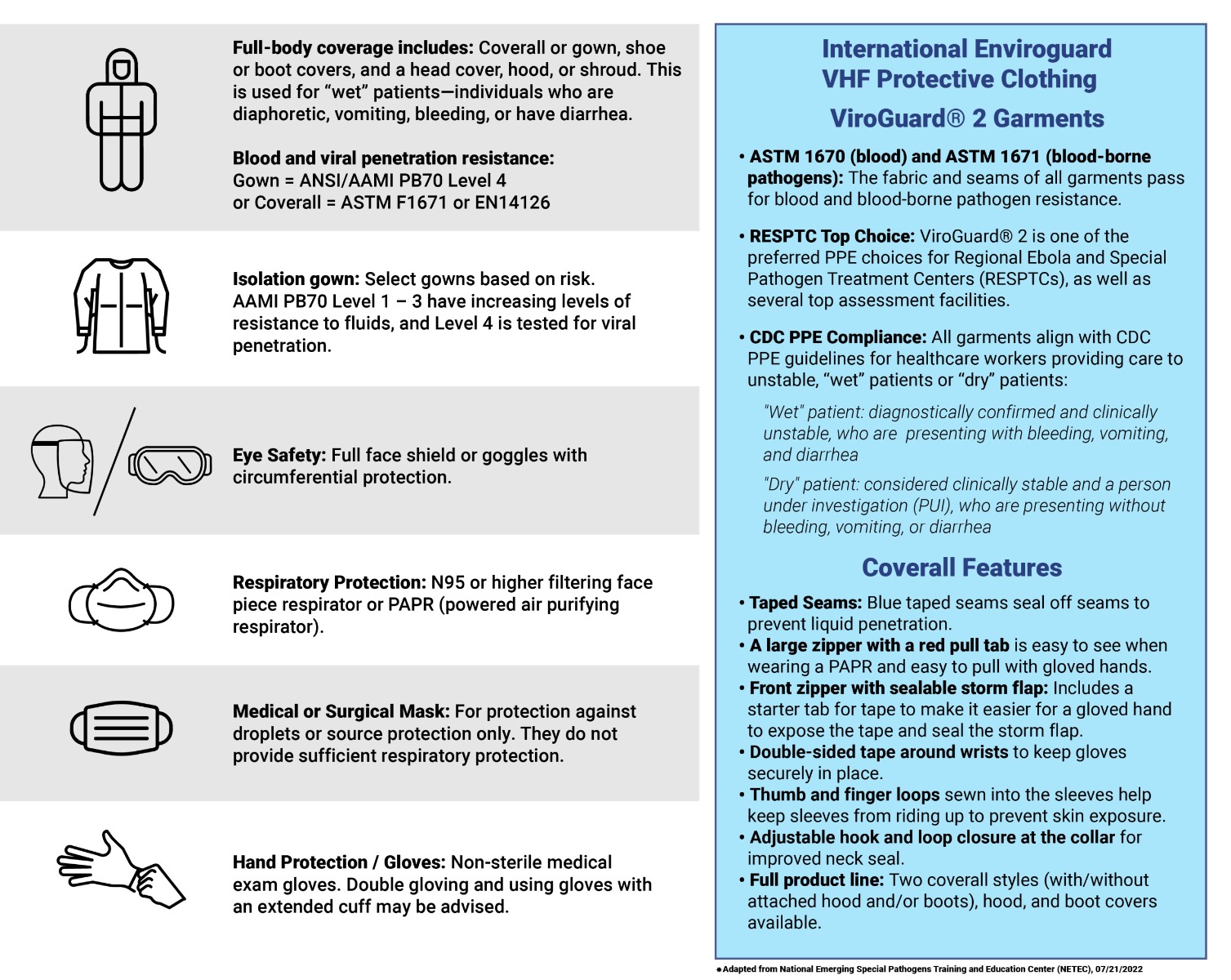
Let's look specifically at the types of PPE recommended for healthcare workers and other frontline caregivers who are helping patients with confirmed or suspected cases of viral hemorrhagic fevers. The CDC recommends the following PPE categories for VHF management:
- Full body coverage (such as coverall/gown, boot covers, and head covers) made with materials that feature specific ASTM and ANSI/AAMI blood and viral penetration resistance levels
- Isolation gown
- Full face shield or goggles with circumferential protection
- Respiratory protection
- Gloves
The specific type of PPE that is needed while caring for individuals with VHF depends on several factors, including the level of risk (e.g., severity and stage of the infectious disease), the type of virus causing the infection, and the type of job duties performed (e.g., endotracheal intubation, lab centrifugation, etc.).
For example, a healthcare worker taking care of a patient with a known or suspected case of Ebola virus disease should adhere to contact and droplet/airborne precautions by using a gown, goggles or full face shield, respirator (N95 or greater) and gloves, and should opt for full body coverage if their patient is in a wet phase of the disease (ensuring all skin, mucous membranes, and clothing are covered).
The CDC further advises that personnel should be directly supervised by a trained observer during the VHF PPE donning/doffing process to ensure all protocols have been followed adequately.
Conversely, for individuals caring for patients with known or suspected cases of Yellow fever or Dengue fever, standard precautions should suffice, including excellent hand hygiene and the use of gloves. For more information, readers are encouraged to refer to the graphs included.
Biohazard Solutions for Your Frontline Team
At International Enviroguard, our industry-leading ViroGuard® 2 meets the stringent standards demanded by the CDC, the American National Standards Institute (ANSI), and the American Society of Testing and Materials International (ASTM) to ensure your workforce remains in full compliance.
Our PPE solutions are made with design features and materials explicitly rated to provide optimal biohazard protection for individuals caring for people with VHFs, including patients who are "wet" (actively bleeding, vomiting, or experiencing diarrhea).
We've also taken steps to optimize durability, comfort, and ease of use to ensure the wearer can maximize their efficiency and productivity without sacrificing their safety. Features include brightly colored zipper pulls that are easy to see even while wearing a full respirator, as well as double-sided tape around the wrists to ensure gloves and sleeves stay in place even during your team's longest, most physically demanding shifts.
All ViroGuard® 2 solutions are fully disposable, helping to ensure your team can keep themselves, their loved ones, and communities safer. We encourage all organizations to ensure their workers are fully trained in how to properly don and doff their PPE, and to establish appropriate PPE protocols within the daily workflow—such as having designated don/doff areas with appropriate signage complete with leak-proof disposable infectious waste containers, hygiene and disinfecting solutions, and more.
Conclusion
Viral hemorrhagic fevers (VHFs) are highly contagious and often deadly infectious diseases caused by a group of viruses including the Ebola and Marburg viruses. While animals and insects are their preferred hosts, viruses that cause VHFs can also infect people and, in some cases, can spread from person-to-person via bodily fluids.
Because of their sporadic, unpredictable, and often deadly outcomes, all VHFs must be handled with extreme caution using strict regulatory and safety guidelines; this includes the correct use of PPE that has been specifically rated to protect individuals against bodily fluids and blood-borne pathogens.
Is your workforce prepared for a future viral outbreak or global health crisis?